Disc prolapse is a diagnostic conclusion often presented to patients after the completion of advanced imaging, such as an MRI. Prolapse amounts to the same definition as a herniated disc. The word prolapse means to slip or be forced out of place, hence the misleading colloquial nomenclature of slipped disc.
Regardless of what name the condition is called, it is one of the scariest and most fear-inspiring of all back pain diagnoses. People hear anything bad about their intervertebral discs and suddenly feel that they have serious and possibly irreconcilable spinal issues. In some scenarios, they may. However, in most, disc abnormalities turn out to be much ado about nothing.
The scope of this article will examine the facts surrounding intervertebral disc pathologies and will also provide some guidance to help patients better understand their options once they are diagnosed.
Disc Prolapse Condition
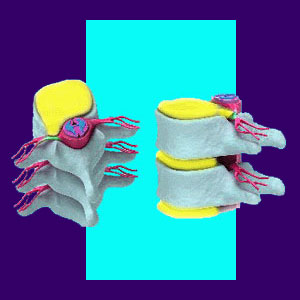
There are many forms of prolapsed disc. The disc might simply bulge, creating an asymmetrical appearance despite the outer wall remaining intact. The disc might also suffer an annular tear and leak some of the inner core of the structure into the body cavity. This condition is often known as a ruptured disc.
The main criteria for the existence of a prolapsed disc is that the integrity of the intervertebral structure has been compromised, creating a bulge, weakness or actual hole in the outer disc wall.
Always be sure to speak to your diagnostician to determine the exact nature and severity of your own disc concern prior to seeking any variety of herniated disc treatment.
Prolapsed Spinal Disc Facts
The very words herniated disc can have a profound effect on any diagnosed patient when uttered by their physician. Intervertebral disc conditions have a well known reputation as extremely problematic disorders to cure.
While it is true that many people suffer with back ache blamed on a bad disc for many years, it is actually quite rare for the disc to be the real source of symptoms in most of these poor misdiagnosed souls.
Actual disc pain is typically reserved for cases of acute trauma and will generally resolve within weeks. The possibility of a herniated disc causing chronic back pain for years or even decades, is very, very slim indeed. Here are some supportive facts:
There is no correlation between the incidence of disc herniation and the existence of back or neck pain.
There are just as many people who do not have any disc issues, yet have intractable pain, as there are who have herniations and chronic symptoms.
There are just as many patients who have no disc issues and no pain, as there are people who have severe disc abnormalities, yet no pain.
Disc Prolapse Conclusions
Before you get yourself all worked up about being diagnosed with a prolapsed disc, take some time to research the condition for yourself. I am sure that you will see that the clinical impression of many disc pain syndromes do not match the expected symptomology of the diagnosis exactly, or possibly, not at all.
I never questioned the diagnosis of herniated discs as the source of my pain and look where it got me… decades of agonizing pain and misery. Had I simply woke up to the facts a bit sooner, I could have saved myself and my loved ones literally tons of pain, suffering and money!
Oh well, for me, salvation came in the form of knowledge, not surgery, drugs or other ridiculous back pain treatments. I used a variety of holistic practices to fully resolve my chronic pain and these techniques eventually became the core foundation for our proprietary pain relief program which has received widespread accolades from care providers around the world.





