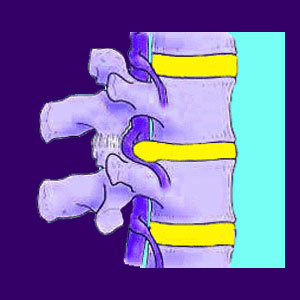
A bulging disc is a type of contained herniation that features an intact outer wall which is only slightly asymmetrical in its protrusion. This means that the inner nucleus of the disc, also called the nucleus pulposus, is pressing against the outer disk wall, named the annulus fibrosus, causing it to bulge outwards. In essence, the disc still maintains the structural integrity of the outer wall. The disc wall has bulged outwards, usually in a specific direction, but has not ruptured, nor leaked any nucleus material.
Disc bulges can be synonymous with herniated discs or may be a distinct term, depending on the preference of the care provider more than the actual characteristics of the disc itself. A great number of doctors and chiropractors use the term bulging disc to represent a minor herniation and reserve the term herniated disc when an actual pocket of asymmetric disc nucleus material forms off the main nucleus structure. However, just as many care providers use the two terms equally and having identical meanings to one another.
This is yet another very confusing aspect of diagnosis for patients to understand. A great number of people get caught up on the semantics of the wording of their diagnostic reports, rather than seeking to understand the far more important prognosis for the condition. This dissertation helps patients to better understand bulging intervertebral discs.
Bulging Disc Concerns
Bulges of the intervertebral discs are extremely commonplace in the human spine. Most bulging discs result from typical spinal degeneration and are not and will never be symptom-generating health issues.
Minor and moderate bulges are viewed as transitory and normal parts of the spine in most instances, especially when they reside in the usual areas of the lower lumbar, lumbosacral and mid to low cervical zones.
Medical research clearly shows that most bulges do not cause pain, do not require treatment and will not necessarily worsen with time. However, it is possible for the disc bulge to worsen or for the disc to rupture. This can be painful, but does not have to be symptomatic. Ruptured discs often stabilize and stop causing pain all by themselves. In fact, sometimes when a rupture occurs, it can actually remove symptomatic pressure on a neurological structure.
In cases where a disc pathology does enact pain or nerve effects, there is no indication that any particular type of disc condition is any more problematic than another. This means that significant bulges, herniations, ruptures, extrusions and sequestrations may all have variable symptomatic potentials based on case-specific criteria rather than the actual classification of pathology demonstrated.
In the case of chronic disc pain, professional medical therapy is sometimes necessary. It should be mentioned that there is a good chance that the treatment will fail to provide relief, regardless of which approach to care is chosen.
Bulging Disc Debate
There are so many examples of disc abnormalities that do not cause any pain. Many of these are discovered by accident when the patient is undergoing a completely unrelated imaging study. Assuming that all disc injuries cause chronic symptoms is a common mistake made by many doctors and therapists. No wonder diagnostic protocol is constantly being revised, urging physicians to never diagnose any spinal irregularity as the source of pain without definitive correlating evidence.
The reality of disc pain is more of a case by case basis. Some injuries can be asymptomatic. Others might cause huge amounts of pain, then heal by themselves. Some disc pain can go undetected for a while, then increase in severity with time. Finally, some pain is chronic and never seems to resolve, regardless of treatment. Disc injuries must be studied carefully in order to rule out other contributing factors to the pain.
Nerve-related pain is sometimes misdiagnosed as stemming from a disc problem. Disease processes and other spinal issues can remain undetected while a bulging disc may be unjustly targeted for blame.
However, one of the more common forms of misdiagnosed symptoms often blamed on herniated discs is psychological back pain. This is the primary reason why so many patients suffer for years or even entire lifetimes. They undergo treatment after treatment for their intervertebral disc issues, yet the pain remains.
Regardless of the mistake in diagnostic evaluation, many victims finally acquiesce to discectomy surgery only to have their pain continue, even after the offending disc material is gone.
Disc Bulge Suggestions
Disc injuries are a huge contributor to the nocebo effect in back and neck pain patients. The average person has heard many horror stories about terrible disc injuries and their effects. We all perceive the spine and discs as being easily injured and difficult to repair. This is simply a fallacy.
Disc injuries do exist, but are rarely the cause for years of chronic pain. In these cases, the poor bulging disc is another innocent scapegoat used to perpetuate the profitable propagation of longterm conservative or drastic invasive back pain treatments.
For further study, I recommend learning more about bulging discs and how each type of herniation may create symptoms through various processes. It is crucial to know that the disc itself will never feel any pain, no matter how destroyed it seems to be. It has no nerve endings itself. The only way a bulging disc can produce any pain is to affect a nerve structure.
Luckily, these neurological interactions will most often provide definitive evidence which can be correlated to the suspected diagnosis to validate or exclude the role of the suspect disc as the true causative mechanism To fully understand this process, consult with your spinal neurologist or orthopedist.





