A collapsed disc is a layman’s term used to describe both degenerative disc disease, as well as some types of herniated discs.
Collapse describes a loss of height, which is typical in both degenerated discs and herniations. The nomenclature of disc diagnoses can be very confusing, so it is crucial that you talk to your doctor to understand the exact nature of any spinal disc pathology.
Disc collapse is a normal process inherent to spinal aging. All of us will suffer some degree of collapse of our lumbar and cervical intervertebral discs as we get older. There is nothing fundamentally painful about disc collapse, but it must be mentioned that this degenerative process is one of the main facilitators of spinal osteoarthritic conditions.
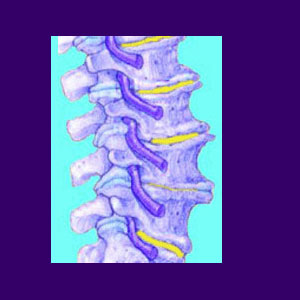
This dialog examines what exactly occurs when a disc collapses, bringing the spinal bones closer together than would be considered normal.
Collapsed Disc Structure
A disc collapse is always thought to be the harbinger of pain and chronic suffering for any affected patient. This is a ridiculous part of medical mythology, since degeneration of the intervertebral disc structures is a normal and universal part of getting older.
Degeneration consists of the dehydration and shrinkage of the normal disc anatomy. This process is not inherently problematic, but does leave the disc susceptible to herniation. Luckily, most bulging discs are also not painful and many exist undiscovered for many years, since they are totally asymptomatic.
When discs do collapse, they create the ideal circumstances for arthritis to occur on the vertebral endplates and within the spinal joints. The closer vertebrae come to one another, the greater the incidence of bony interactions which can result in general arthritic debris and even osteophyte formation.
Collapsed Spinal Disc Concerns
Generally, medical science views degenerated discs and herniated discs as possible sources of discogenic pain, spinal stenosis and foraminal stenosis enacting pinched nerves. While these conditions might exist in some rare patients, they certainly do not describe the experience of the average person affected by degeneration of the spinal discs.
In fact, most discs deemed to be pathological are misdiagnosed as the source of any severe or chronic back pain, leading the patient to attempt many unsuccessful herniated disc treatments. It is no surprise that a variety of seemingly appropriate therapy options fail, since the vilified disc is innocent and coincidental to the painful complaint.
Collapsed Disc Guidance
If you have pain from a herniated disc enacted by a traumatic back injury, you should expect to enjoy relief in 6 to 8 weeks. Ongoing disc pain is rare, even if the injury is severe. Degenerative disc disease and intervertebral collapses which result from the normal degenerative processes should not be painful at all or mildly symptomatic at the worst. Patients whose back pain is blamed on DDD or a non-injury related herniation must be careful that they are on the right track when seeking treatment. This was my exact situation and I endured 18 years of failed therapies, since my pain was grossly misdiagnosed.
If your doctor has used the diagnostic term disc collapse to describe your spine, be sure to discuss with them the exact definition that they intend to convey from the verdict. Some doctors will describe collapsed spinal discs casually, taking for granted that the patient understands that this is a normal and universal event to experience. Meanwhile, the patient might be terrified to learn that they have a collapsed spinal spacer in between their vertebrae.
On the other hand, a doctor might play up a collapsed spinal disc diagnosis, making it seem like a terrible thing which will surely cause pain. Clarify these points to be sure of your doctor’s intent and also to better understand the degree of collapse in the disc structure itself.




