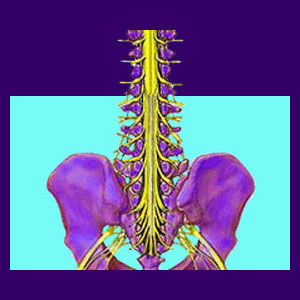
A compressed nerve root is also known as a pinched nerve and typically describes structural impingement of a spinal nerve within the backbone anatomy. This structural compression can occur for many reasons and can even take place far away from the spine, along one of the peripheral branches of the nervous system.
Compression is defined as physical force applied to the nerve, disallowing it to function normally in sending and receiving neurological signals. It should be noted that although compression might seem to be enacted due to mechanical issues, it is often misdiagnosed due to identical pain patterns caused by regional ischemia.
This discussion provides an overview of pinched nerves in the spine, outside of the immediate spinal anatomy and conditions that mirror pinched nerves in their expressed symptomology.
Spinal Compressed Nerve Root
Nerve roots exist in the spine and branch out to form a neurological network throughout our anatomies. Nerve roots eventually form the body’s major nerves and all their peripheral branches.
Anatomical compression of a spinal nerve root can create some big problems, including pain, tingling, weakness and numbness in the area served by the affected neurological structure. This event is most common in the lumbar spine and cervical spine, although it can occur anywhere in the vertebral column.
It is crucial to understand that pinched nerves are a very widely used back pain scapegoat. This means that nerve compression is often diagnosed by speculation, when in fact, the pain is due to a completely different process. This occurs often in the diagnoses of spinal stenosis and foraminal stenosis, especially when enacted by a herniated disc or arthritic osteophyte.
Muscular Compressed Nerve
There are actual soft tissue enacted nerve compression syndromes which occur within the spinal anatomy, as well as quite some distance away from the spine. Piriformis syndrome is a perfect example of how a muscle can clamp down on a nerve and create symptoms identical to a spinal pinched nerve. The sciatic nerve is the typical target of these pain syndromes, although thoracic outlet syndrome is also a diagnosis on the rise.
Muscular nerve compression is even less common than spinal nerve root impingement and the vast majority of cases are grossly misdiagnosed, as well. However, when they exist, the root process may also be due to ischemia causing the muscle to tighten, go into spasm and eventually affect the victimized nerve.
Ischemia Mimicking a Compressed Nerve Root
Oxygen deprivation can cause symptoms which perfectly mimic structural compression anywhere in the body. Ischemic pain syndromes are an epidemic menace in today’s healthcare industry with the majority of treatment-resistant conditions falling into this category.
Ischemia is rarely correctly identified as the actual source of symptoms, since it is most often driven by a psychosomatic process and diagnosis of these circumstances goes against the Cartesian philosophy (and therefore the profit margin) of most of the back pain industry.
Compressed Nerve Root Evaluation
Pinched nerves happen. They can really hurt. However, they typically resolve either by themselves or with appropriate treatment. Persistent pain from a compressive neuropathy is not typical, since continuous impingement on any neurological structure will cause that structure to stop signaling completely. The result is objective numbness; not chronic pain.
If you have unresolved back pain blamed on a pinched nerve or other radiculopathy condition, you should consider the possibility that your pain may be enacted by oxygen deprivation.
Luckily, the treatment for mindbody ischemia is simple to enact and generally highly effective. Knowledge therapy is likely to be the best course of action, based on its efficacy and complete lack of risk and cost.





