A disc protrusion is yet another diagnostic name for a general herniated disc condition. The ever-growing number of terms used to identify this common spinal abnormality certainly does a fair share to confuse diagnosed patients, since many do not completely understand the implications of their specific intervertebral conditions. I always recommend talking to your doctors to better classify the type and severity of any diagnosed disc pathology. This is the first step towards successful treatment, if needed, and is certainly one of the best ways to dispel the nocebo effect of the diagnostic process.
This essay explains intervertebral protrusions and their possible effects on the greater vertebral anatomy.
What is a Disc Protrusion?
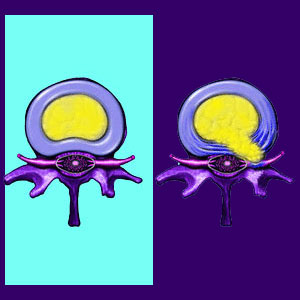
Protrusion indicates that part of an intervertebral disc is bulging beyond its normal size and shape. This bulge might be completely asymptomatic or may create some degree of pain and related symptoms, depending on the size, direction and destination of the bulge.
In most circumstances, protrusion is a term used to describe a contained bulging disc in which the integrity of the outer disc wall, called the annulus fibrosus, remains intact. Sometimes, a ruptured disc is also said to cause a protrusion, meaning that the nucleus pulposus has spilled out of the outer disc wall, creating an extrusion of nucleus material which may or may not cause symptoms identical to or different than a contained herniation. Often, a ruptured protrusion is blamed for enacting chemical radiculitis in the surrounding neurological tissue.
Protruding Disc Diagnosis
Disc protrusions can be seen via diagnostic imaging like CT or MRI. They will not show up well, if at all, on x-rays and certainly can never be accurately diagnosed via physical exam alone. Despite antiquated mythology, there is no sure way to diagnose a herniation through any physical movement, such as the often utilized straight leg raising test.
Just because a protrusion exists, does not mean that symptoms need be present. In fact, most bulging discs are not painful and cause no problems whatsoever. Some bulges are painful for a short time, typically 2 to 8 weeks, especially when they result from considerable trauma. It makes sense that most back injuries are painful, regardless of whether they cause a herniation or not.
Many times, a protrusion is blamed for pain which is actually caused by a completely different structural or psychosomatic causation. In these instances, the protrusion is simply a back or neck pain scapegoat, since it is coincidental to the painful complaint. Remember, herniated discs are some of the most common abnormalities in the human spine.
Disc Protrusion Ordeal
I was diagnosed with 2 lumbar herniations in my early 20’s. I was very scared of the damage these discs would do to my spine and this fear was intensified by the diagnostic nocebo effect imparted by some of my caregivers. Very rarely do doctors inform the patient that the existence of a herniation does not mean that pain will inherently be present. Doctors will also rarely tell you that herniated discs exist in most people, with or without back pain.
I have never heard a doctor tell of the diagnostic guidelines which warn them not to diagnose any back or neck pain based on some structural spinal abnormality, unless a definitive causative process can be ascertained and proven.
Disc conditions have a fearsome reputation, but seldom live up to their undeserved fear factor. To learn the full story about why many herniated discs do not pose any health risks at all, consider using knowledge therapy to improve your understanding of the spinal anatomy and move past the fear inherent to the diagnosis of a protrusion.




