Facet syndrome is one of the terms used to describe symptomatic deterioration of the spinal zygapophysial joints. Being that facet arthritis is often diagnosed by exclusion, or anesthetic injection, many errors can occur during the process, possibly leading the patient the wrong way in their quest to find relief.
Facet joint syndrome is a popular scapegoat explanation for chronic back ache when there is no evidence of a more definitive structural pathology to take the blame. While facet joint degeneration is easy to see on any diagnostic film study, many patients do not know the simple fact that the process is completely normal in the human vertebral column. Doctors conveniently do not typically mention this basic truth during most diagnostic consultations.
This essay details the diagnostic process for facet joint pain syndromes and teh many problems that are typically encountered by patients.
Facet Joint Syndrome Diagnostic Process
Normally, preliminary spinal X-rays are taken, followed by a CT scan or MRI. Remember, facet joint degeneration is normal, especially in older or active people. Therefore, facet joint syndrome is common to find in back pain patients. Facet syndrome is also common to find in people with no back pain.
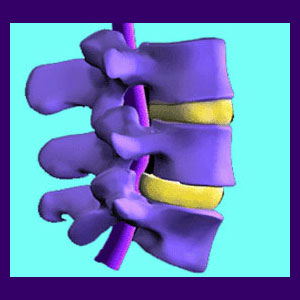
Imaging studies will look at the actual vertebral bones first. Signs of facet syndrome will be noted. Next, indications of neurological impingement, also known as pinched nerves, will be investigated. Sometimes, the facet joint degeneration can lead to the growth of bone spurs, which might compress a spinal nerve root. The possibility for mechanical pain will also be evaluated.
Once all the data is in, the evidence of whether or not facet joint arthritis may be causative or contributory to the symptoms should be quite clear. If no other source of pain is obvious, facet hypertrophy is one of the old stand-bys that can always be blamed for causing agonizing symptoms. However, in many cases, there is little proof of the facet joints being directly causative for pain, so additional steps might be taken to almost forcibly implicate them so the patient can be put into treatment.
Anesthetic Diagnosis of Facet Joint Disease
One of the most popular ways to pinpoint facet joint syndrome as the cause of pain is with an anesthetic nerve block. Anesthetic is injected directly into the capsule of the facet joint under live X-ray. If the pain is relieved, then the facet joint is usually blamed for the symptoms. This is where the entire diagnostic process often goes awry.
Research points out that the anesthetic dose is often up to 100 times too large to numb just that individual joint. The anesthetic will spread and can affect all the spinal nerves in the area. This basically blocks pain from any cause in that spinal level. Sometimes multiple spinal levels are numbed. Obviously, this is not a reliable diagnostic technique, but makes a great smoke and mirror routine when a doctor wants something substantial on which to blame the pain.
Anesthetic evaluation and diagnosis can be useful when performed objectively and by a true expert. However, in some cases it is clearly being abused as a modality to convince a patient of a mistaken diagnosis and get them into profitable care.
Facet Syndrome Diagnosis Final Thoughts
Don’t be surprised if you are told that you have facet joint degeneration. I have it and so do many people. As we age, we will all have it to one degree or another. Be sure to tell your doctor that they have it too. Do not let some exaggerated mental picture of your poor vertebrae rubbing violently together cause you to have worsened symptoms. Remember, this diagnosis can cause a very powerful nocebo effect.
Always take time to research any diagnosis you receive and be active in learning all you can about the condition. You would be surprised how many patients can prevent misdiagnosis simply by reading about their condition and finding obvious holes in the theory of what is actually causing pain.
Many patients find that their symptoms do not correlate in location or expression. Others discover another potential cause which makes more sense in their specific circumstances. Often, these patients are right and are justified in questioning the diagnostic blunders.
At the very least, I always recommend seeking a second opinion before getting involved in any ongoing treatment program. If surgery is recommended, I up the advice to get at least 2 more opinions before even considering that potentially risky path.




