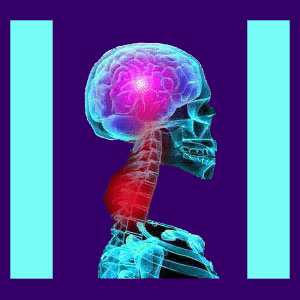
Neck pain from a herniated disc is a common diagnostic theory used to explain chronic symptoms in the cervical spinal region, as well as discomfort that might radiate into the upper back, shoulders, arms, hands or fingers.
Cervical herniated discs are extremely common, especially at C5/C6, C6/C7 and C7/T1. This is because the extreme mobility of the neck increases the rate of disc deterioration and the considerable weight of the head places a substantial burden on the cervical vertebral column.
Many of the structural changes associated with cervical bulging discs are nothing to be concerned with, since most intervertebral abnormalities are completely asymptomatic. However, in rare instances, a herniated disc can enact pain and other troublesome symptoms through cervical spinal stenosis, foraminal stenosis or even chemical radiculitis.
This dissertation examines neck pain that is caused by intervertebral disc pathologies. We will detail the exact reasons why neck pain may occur from a disc irregularity, as well as balance the conversation by explaining how most herniations are not the source of any pain or neurological expressions.
Neck Pain from a Herniated Disc Processes
Herniated discs are not typically painful. This is because most herniations do not influence any nerve tissues, so they can not generate pain messages. Intervertebral discs do not feel pain, as they have no internal nerve endings. The only way they can cause pain is to affect the spinal cord or the spinal nerve roots.
Pain might exist when a disc impinges on the spinal cord within the central canal space. This process is known as transient spinal stenosis, since the canal narrowing is enacted by a soft tissue condition and not an arthritic process or other permanent causation.
Pain might also occur when a herniation impinges on one of the cervical spinal nerve roots, either within the lateral recess, or more commonly, in the foraminal space, where the root exits the central canal. This latter process is called transient foraminal stenosis and can create a condition known as a compressive neuropathy, more often called a pinched nerve.
In other cases, a ruptured and leaking disc may be blamed for creating pain due to irritation of surrounding neurological tissue; a process called chemical radiculitis.
In extremely rare occasions, discs may be implicated to suffer from a diagnosis known as discogenic pain. In these cases, the actual tiny nerves which supply with endplates of each disc structure are thought to be involved in causing the painful complaint. This last theory is rather controversial, since even when suspected to exist, the symptoms rarely align with the clinical expectations.
Herniated Disc Neck Pain Diagnosis and Correlation
Simply demonstrating a cervical herniation does not mean that symptoms are linked to the disc abnormality. In fact, the overwhelming majority of disc irregularities expressed throughout the spine have been proven to be innocent and asymptomatic.
Disc abnormalities must be studied carefully and thoroughly, using all the testing methods that are available to the patient. MRI and CT scans are helpful, as are discograms and nerve conduction testing.
Furthermore, clinical correlation of symptoms is a crucial part of the diagnostic process, but is often overlooked. In many patient profiles, we see obvious problems when comparing the actual pain with the working diagnosis. This is because the locations of symptoms often do not correlate to the nerves that are suspected of generating the pain signals.
We typically see patients who have foraminal herniations on the left, but express symptoms on the right. We see patients theorized to have compressive neuropathies, yet have symptoms in areas not served by the affected nerve. We see patients who have severe pain and a tiny herniation that is obviously not affecting the cord or nerve roots, yet is deemed responsible for the agony nevertheless.
Unless a pathological process can be positively identified, physicians are advised to discount the disc as a causative factor in the pain complaint and continue to evaluate the patient to find the actual symptomatic source process.
Unfortunately, many doctors and chiropractors assume that any structural abnormality is inherently the cause of pain. This presumptive misdiagnosis accounts for the terrible treatment results suffered by millions of cervical herniation patients. Remember, even if the disc protrusion is successfully resolved, the pain will continue if the condition was never the origin of symptoms.
Neck Pain from a Herniated Disc Assistance
Chronic neck pain is a truly debilitating condition. It is also the second most prevalent dorsopathy concern, beaten only by chronic lumbar back pain. The majority of chronic neck pain complaints are attributed to disc pathologies, often without any evidence of a relationship between the structural changes and the symptoms.
The good news is that actual structurally-motivated cervical disc pathologies generally respond well to appropriate treatment and resolve in due time. In fact, many herniations will heal all by themselves, as the bulge subsides and organically relieves pressure on the affected nerves.
Pain syndromes which defy medical and complementary medical care are almost always misdiagnosed. We see many patients who have attempted all manner of herniated disc treatments, ranging from nonsurgical decompression to cervical discectomy to cervical artificial disc replacement to spinal fusion. Regardless of the extreme nature of the therapy utilized, many patients still have symptoms, and in some post-surgical patients, the pain is actually worsened.
The lesson to be learned is that time must be taken during the diagnostic process. Too many patients are rushed into the treatment phase prematurely and suffer unsuccessful conservative therapies leading to failed surgeries.
Our advice? Do not allow any doctor to scare you into treatment until you are certain of the accuracy of the diagnosis and have elicited at least 2 more qualified medical opinions confirming the proposed therapy recommendation. This active involvement will better any patient’s chances of finding lasting relief from herniated disc neck pain.





