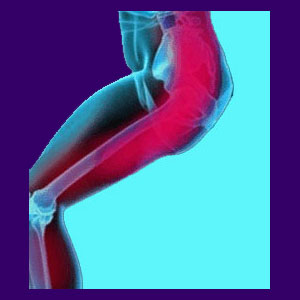
Piriformis pain can create an agonizing set of sciatica symptoms classically diagnosed as piriformis syndrome. This is a highly controversial condition, with heated arguments raging throughout the medical community concerning the actual validity of the diagnostic methods and conclusion. Regardless, the diagnosis is on the rise and accounts for a sizeable percentage of patients suffering with sciatic nerve symptoms.
The one thing which is universally agreed upon in piriformis syndrome is that symptoms are elicited by compression of the sciatic or pudendal nerves. However, what remains under debate is the basic reason why the piriformis constricts this largest anatomical nerve and more importantly, how to stop it from doing so.
This narrative discusses how and why the piriformis muscle might be involved in causing chronic buttocks and leg pain problems in some patients.
Piriformis Pain Causes
There are certain theorized contributing factors to the development of piriformis syndrome:
Genetic factors contribute due to the actual patient’s anatomy. Some people are born with their sciatic nerve passing through the piriformis muscle, rather than well below it. Other genetic factors regarding the size and shape of the piriformis and surrounding muscles seem to contribute to the development of painful symptoms. However, this is by far not a universal conclusion, since many patients do not demonstrate these factors, yet are still diagnosed with symptoms nonetheless.
Sitting for extended periods of time is an exacerbating factor for most patients. Sitting with anything in the back pocket of the pants is another possible contributor to this syndrome.
General activity level seems to play a part in the development of piriformis syndrome. Generally active people are less susceptible to piriformis symptoms than sedentary individuals.
Piriformis Pain Syndrome
Many doctors do not believe this condition even exists. Others dedicate their entire practice focus to it. I have seen enough evidence to believe that piriformis syndrome does indeed affect some unfortunate patients.
However, I also have seen many patients suffering with cases of oxygen deprivation back pain that are misdiagnosed with piriformis syndrome. Oxygen deprivation pain is far more common and should always be thought of first when a patient presents piriformis syndrome symptoms.
Remember, these diagnoses are interrelated since the very reason the muscle might be chronically tight may certainly be ongoing regional oxygen deprivation.
Resolving Piriformis-Related Pain
I like the fact that in many diagnosed cases of piriformis syndrome, the usual spinal scapegoats which may have traditionally been blamed for causing the symptoms have been exonerated. However, I do not like the structural obsession with injury so often illogically included with the piriformis diagnosis. Sure, when the nerve-through-muscle irregularity exists, there may be some credence for the idea that the design of the muscle itself causes the pain. However, what about the vast majority of patients diagnosed with piriformis syndrome who do not demonstrate this abnormality?
I would like to see logic better applied here and suggest that all doctors treating piriformis pain do their own research as to ischemia being the possible source. This regional process will continue basically unchecked if never targeted for treatment.
This potential source of suffering makes lots of sense when you consider the transient benefits offered by so many piriformis therapy options which increase circulation to the affected area. Think about it…




