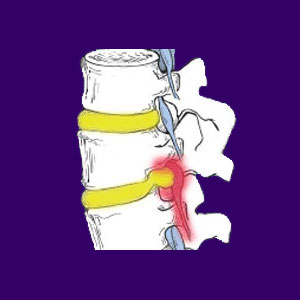
A prolapsed disc is another commonly used medical name for any variety of herniated disc. This particular description is typically used when the inner nucleus pulposus bulges against the outer annulus fibrosis, potentially causing nerve root impingement. Disc prolapse has a bad reputation as a symptomatic and chronic condition, but it is clear from medical evidence that this malevolent scenario is the exception, not the rule. Prolapses of the intervertebral spacers are actually unbelievably commonplace. Although bulges are officially still classified as spinal abnormalities, the large number of people with asymptomatic spinal herniations might beg to differ.
The overwhelming majority of people have one or more bulging or ruptured discs in their neck or low back, yet most do not even know it. This is because these herniations occur due to normal degenerative processes and do not cause any discomfort now or ever. Of course, this is not to say that herniations can not be problematic. They certainly can be troublesome, particularly when enacted by violent trauma. However, the circumstances by which disc pathologies can create chronic pain are limited and represent the gross minority of disc irregularities.
This essay focuses on clarifying intervertebral prolapses in the spinal anatomy, more commonly known as herniated discs.
Prolapsed Disc Condition
Most herniated discs do not cause any significant back pain symptoms. Some significant disc injuries are painful when they first occur, but resolve quickly and completely in a matter of weeks. Most do not require any special care or treatment.
Some disc conditions might cause transient spinal stenosis symptoms or pinched nerves, although long-term pain associated with these instances is rare. Remember, as previously mentioned, disc prolapse is actually a very common spinal abnormality and a sizeable percentage of adults demonstrate one or more bulging, ruptured or degenerated discs in their spines, but suffer no ill effects.
Disc Prolapse Diagnosis
While X-rays can show a narrowing of disc tissue, they can not confirm a disc herniation. Only a diagnostic test, such as an MRI or CT scan, which is capable of producing a view of soft tissues, can accurately diagnose a disc problem.
Many slipped discs are found during routine MRI testing for a completely unrelated reason. The patient was never aware of the disc condition, since the disc never caused them pain.
Remember that degenerative disc disease is a normal part of the aging process and is also a contributor to disc prolapse. Therefore, disc herniations are also a normal part of the aging process for many healthy adults.
Analysis of a Prolapsed Disc
Disc conditions are used as back pain scapegoats more than any other spinal causation. While the back pain industry continues to aggressively treat herniated discs, the results of said treatments are often poor and barely control the symptoms, forget about rectifying the actual cause of the pain.
In patients who suffer from treatment-resistant disc pain, the diagnosis is often incorrect. Misdiagnosed back pain conditions are the number one reason for patients to suffer year after year without finding a real cure for their misery. If you have a diagnosed disc abnormality, which has not responded to appropriate treatment, I urge you to consider that the problematic disc might not be a concern at all. It might merely be taking the blame while all along some other physical or psychogenic causation is really enacting all your agony.
Remember that curing any form of back pain is virtually impossible without an accurate diagnosis. Never take for granted that your diagnosis is correct no matter how much you like your doctor or how respected they might be. Every doctor has the potential to make mistakes. Given the epidemic occurrence of misdiagnosis, it seems that some doctors get more diagnostic theories wrong than they do right.




