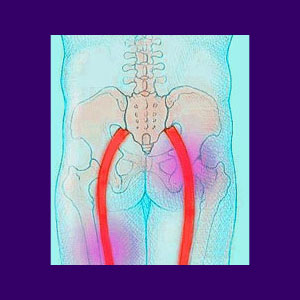
Sciatic nerve pain can come from several different spinal conditions, as well as some non-spinal structural concerns and regional processes. True sciatica is due to a causation in the lower spine, as opposed to the SI joint or piriformis muscle.
5 sets of nerve roots exit from the lower spine and join together to form the sciatic nerve. When one or more of these nerve roots are compressed prior to the main nerve being formed, the signal going to and from the sciatic nerve will be interrupted. If the nerve signal is interrupted or altered, painful symptoms may begin.
The scope of this article will focus on the potential spinal reasons for sciatica to exist, including most of the usual culprits and a few which are rarely considered. This article will not detail pseudo-sciatica, which is a diagnosis describing identical symptoms enacted by a non-spinal causation.
Sciatic Nerve Pain Causation
The following are all spinal conditions which can compress or otherwise affect a lumbar or sacral nerve root, leading to a painful sciatica expression:
Herniated discs can cause sciatica pain. A bulging disc can press on one of the nerve roots and interrupt the signal to/from the sciatic nerve. This is especially common in the L4/L5 and L5/S1 levels. This is a classic example of a pinched nerve. It should be noted that a large percentage of the population have herniated discs, but experience no symptoms at all. Even when discs do compress a nerve root, the effects may be temporary and many of these circumstances resolve without professional care.
Degenerative disc disease can cause intervertebral discs to flatten and bulge. This process brings the vertebrae closer to one another, narrowing the foraminal spaces through which the nerve roots must exit. Remember, that disc degeneration is normal and does not mean pain is caused by the narrowed disc spaces.
Spondylolisthesis is when a vertebra slips forward and out of alignment with the rest of the spine. This can potentially cause pain due to compression of one or more spinal nerve roots. Remember that many people have mild to moderate versions of this condition and remain symptom-free.
Spinal stenosis can constrict the actual spinal cord or nerves in the central canal. This condition can lead to treatment-resistant sciatic pain, no matter were it occurs in the vertebral anatomy. Remember that stenosis is a normal part of aging and most people do not suffer any ill effects from average levels of canal narrowing.
Spinal curvatures, such as hyperlordosis, hypolordosis, hypokyphosis, hyperkyphosis and scoliosis can all entrap nerve roots within a decreased curve, typically at the apex.
Osteoarthritis in the spine can close off the foraminal openings, constrict the central canal or simply affect nerve roots directly, usually through compression enacted by osteophytes. All of these processes can lead to sciatica symptoms.
The Factual Bottom Line on Sciatica Pain
Sciatica is not a condition in itself. It is simply the symptom of a spinal problem somewhere else. It might affect the legs predominately, but the cause is in the backbone.
Being that the source of pain might exist outside the lumbar spine, proper diagnosis may be difficult. I can not even begin to tell you how many patients with cervical or thoracic stenosis demonstrate sciatica pain syndromes. Worse still, so many of the above spinal issues are usual in the lumbar anatomy of adults and might not cause any pain. However, they may be mistakenly blamed for the sciatica, even though they are innocent.
When you account for all these factors, it is no wonder that sciatica is such a difficult condition to cure. After all, in so many patients, the true cause is so incredibly subjective and open to diagnostic interpretation.




