Spinal cord stroke, also called ischemic myelopathy or spinal cord infarction, describes an oxygen deprivation event that affects the spinal cord, rather than the brain. Spinal stroke is uncommon, but can cause dire symptoms, including terrible pain, paralysis, incontinence and death.
There are different varieties of cord infarction and many possible causative and contributory factors that create this dreaded event. Treatment can be successfully rendered if the patient is lucky enough to get emergency medical intervention immediately and is fortunate enough to have the condition properly diagnosed in a timely manner.
Spinal cord stroke is a condition that is far more commonplace among people with particular risk factors. Therefore, the scope of this essay is to warn patients who are at risk that they might have an increased chance of suffering cord infarction, so as to prepare them for the possible onset of sudden symptoms.
Spinal Cord Stroke Explained
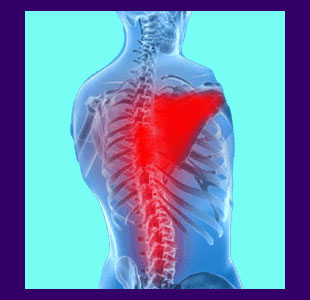
The spinal cord receives blood supply just like every other bodily tissue. In fact, the vascular supply to the spinal cord is rich and abundant, as one would expect, given its importance to human functionality. Two major vessels provide the blood and nutrition that the spinal cord requires in order to function and these are the anterior and posterior spinal cord arteries.
Cord infarction describes a condition of cellular death, specifically where one or more arteries are blocked, partially or wholly, causing the spinal cord to suffer ischemia, also called reduced oxygenation, due to insufficient blood flow. The spinal cord cells are some of the most sensitive in the entire body, as are virtually all neurological tissues, and therefore suffer terrible consequences from even low levels of reduced oxygenation.
When a spinal cord cell does not receive oxygen for an extended time frame, it will die. Since cells in the spinal cord do not necessarily rejuvenate, the resulting loss of tissue and functionality may be permanent, if the patient is lucky enough to survive the initial onset of acute symptoms.
Ischemic Myelopathy Causes and Contributors
Spinal cord infarction is a rare event. Typical cerebrovascular accidents (CVAs) outnumber spinal cord ischemia conditions by a ratio of 99 to 1. In essence, spinal stroke accounts for only about 1% of all reported stroke occurrence. However, there are known risk factors that might predispose a particular individual towards suffering a spinal cord or conventional stroke including any or all of the following:
Atherosclerosis is certainly the most common cause of stroke, including spinal cord infarction. Pathological buildup of plaques within the aorta or spinal cord arteries is a major causation of infarction within the central nervous system components.
Arterial trauma to the spinal cord arteries, or the major arteries of the heart, can contribute to stroke. A history of heart surgery is often a significant cause of arterial damage.
Aortic aneurism is a major component of many stroke events. The chances of suffering an aneurism are increased by additional risk factors, including diabetes, certain infectious processes, old age, being overweight, having high blood pressure or being a substance abuser.
Certain diseases increase the susceptibility towards spinal stroke.
Spinal pathologies can affect arterial components in rare instances, causing structural compression or direct trauma. Extreme intervertebral protrusions, significant atypical spinal curvatures, ligamentous hypertrophy and various spinal arthritic processes might all play roles in the development of arterial injury and subsequent spinal cord infarction.
Spinal Cord Stroke Symptomology
Symptoms of cord infarction often mimic other severely acute causes of back and neck pain, making diagnosis a difficult proposition in some instances. The existence of advancing age and additional risk factors are the usual indicators of possible spinal stroke versus some other causation, as is the rapid timeline of onset. Symptoms of cord infarction might include any or all of the following expressions:
Patients typically experience severe pain in the affected region of the spine, although generalized severe back or neck pain is also a common citation. This pain often does not last long, as it is soon replaced by objective total loss of neurological signal. Onset of neurological deficit usually occurs within an hour to two hours, aiding in diagnostic evaluation.
Patients will usually lose motor functionality in the limbs that are innervated below the affected spinal level first, then experience diminished sensations of pain and temperature. Complete paralysis of affected limbs is commonplace. Once again, onset is rapid, helping to ascertain the nature of spinal stroke versus other types of causations, such as compressive cauda equina syndrome or spinal stenosis.
Patients often report a loss of ability to retain urine or feces or the inability to void the bowels or bladder. Incontinence is a more telling indication, since it occurs rapidly and therefore can assist in diagnostic confirmation of spinal cord infarction.
Spinal Cord Infarction
If the diagnosis is confirmed quickly and the patient can receive targeted treatment, survival rate increases and permanent loss of neurological functionality might be minimized. Unfortunately, many patients are not diagnosed quickly, or at all, leading to complications of spinal stroke, including death, permanent paralysis or other serious disorders.
To learn more about spinal stroke, or to determine if you demonstrate heightened risk for its occurrence, please consult with your physician and have them correlate your personal health condition to known onset contributors.





