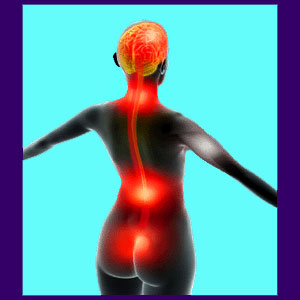
Spinal meningitis is a serious infection of the spinal membranes, including any or all of the dura mater, arachnoid mater or pia mater. These layered protective sacs surround the central nervous system components, including the brain, the spinal cord and the spinal nerves. Within the membranes exists the cerebral spinal fluid or CFS. This fluid allows the infection to spread to all the most vital areas of the central nervous system, which causes serious consequences to the health of the individual.
Meningitis comes in several distinct forms and causations, often complicating diagnostic efforts and slowing the treatment process. Since all virtually forms of meningitis have the potential to become life threatening, medical science has risen to the challenge of finding effective approaches to diagnose and treat the condition based on expressed symptomology and confirmation testing.
This focused dialog explores the various diseases included in the meningitis diagnosis. We will examine the causes of meningitis, the symptoms of meningitis and the ways that modern medicine battles the condition once it strikes.
Spinal Meningitis Causes
Meningitis simply describes a category of conditions that involve inflammation of the spinal meninges and infection of the CSF. There are actually several distinct forms of meningitis, all of which require different treatment techniques:
Meningitis is most commonly caused by a virus. Viral meningitis is considered to be the least serious, although some cases can still pose significant health threats to people in high risk categories.
Meningitis can be causes by fungal infection, particularly in patients with less than optimal immune functionality.
Parasites can infect the spinal membranes and cause meningitis, as well. Parasitic meningitis varies in severity and treatment protocol. Luckily, this form of the disease is mostly confined to underdeveloped parts of the world and is rarely seen in most modern medical environments.
Meningitis can be caused by bacterial infection of the meninges and/or CSF. Bacterial infection is known to be difficult to treat and also provides some of the worst possibilities for permanent injury to the sensitive central nervous system components.
It is a little known fact that there are forms of meningitis that do involve spinal meninges inflammation, but do not involve any infectious process. These types of the disease can be associated with cancer, allergy or various types of autoimmune disease.
It should be noted that spinal surgery is a cause and contributor to many cases of meningitis each and every year. This provides yet another reason to be wary of surgical recommendations, unless an operation is truly unavoidable.
Spinal Meningitis Symptoms
Each type of meningitis produces unique symptomatic expressions that might vary from patient to patient. However, there are several rather common symptoms that are found within multiple types of meningitis infection:
Nuchal rigidity describes spasmodic neck stiffness wherein the neck is so tight and often forced into very unnatural and uncomfortable positions. Some patients merely demonstrate a feeling a stiffness, but do not display any involuntary spasm in the musculature of the neck region.
Fever is virtually universal and might become very high in some patients. The fever alone can become a medical emergency when it reaches the limits of human endurance and can cause death or lasting injury to the brain or body.
Many patients demonstrate an acute sensitivity to bright light. Sensitivity to loud or sudden sounds is also commonplace.
Patients might lose consciousness, become semi-conscious and incoherent, or seem to be in a daze. Patients might experience seizures or fits while conscious or unconscious.
Patients might complain of seemingly illogical sensations in the arms or legs, such a severe tingling or numbness. Cold appendages are also common manifestations of meningitis. Reduced or lost circulation might occur in the arms, hands, legs or feet of some patients, unilaterally or bilaterally, and might lead to tissue necrosis and gangrene.
Rashes are commonplace and particular forms of rash help to diagnose specific forms of meningitis.
The inherent inflammation of meningitis is one of the biggest dangers, as it can create spikes in intracranial pressure and therefore increase the chances for brain damage. This inflammation is not generally a result of the infectious process itself, rather than a direct result of the body’s own immune response.
Permanent damage is often done to the brain or body of patients who do not receive adequate treatment, yet still survive the acute phase of the infection. Even given ideal medical intervention, patients still have the possibility of suffering lasting physical or cognitive deficits from severe meningitis infections.
Spinal Meningitis Prevention and Treatment
The best ways to prevent spinal meningitis are through the use of sanitary practices, such a hand washing and through the implementation of basic immunizations, most often given during childhood.
Some demographics demonstrate heightened risk for developing meningitis, including people who have suffered severe head injuries, people who have received spinal or cranial surgery and people who use certain type of implants, including cochlear implants. Pregnant women are at increased risk, as are their fetuses. School-aged children represent a large percentage of meningitis patients yearly. Finally, people with compromised immune systems certainly present some of the worst risks for developing various types of meningitis.
Meningitis should always be diagnosed and treated by a qualified emergency medical facility, such as a hospital. Time is of the essence when suffering from meningitis, so it is always best to evaluate any suspected case immediately for best patient outcomes.
Viral meningitis is generally allowed to resolve on its own, although anti-inflammatory agents and supportive care are typically provided.
Bacterial, parasitic and fungal meningitis generally require specific medical therapies and these interventions range greatly, depending on the exact source of infection. The earlier a verified diagnosis can be reached, the better the patient’s odds for a complete recovery.
For more information about spinal meningitis, please speak to your physician or an infectious disease specialist.





